Our paper entitled “Probing consciousness in a sensory-disconnected paralyzed patient”, showing how advanced EEG methods can help clinicians to probe consciousness in an extreme case, - named “Deafferented Locked-in Syndrome”, - is available online on Brain Injury.
free postprint available
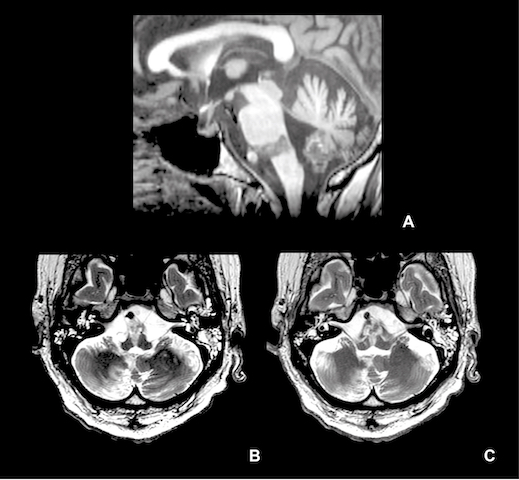
Figure 1. MRI in sagittal T1-weigthed (A) and axial T2-weighted acquisitions (B, C). There is a localized ischemic lesion at the upper part of the medulla oblongata and lower part of the pons, including the cortico spinal tracks and nuclei of the VIIIth nerves. Bilateral filling of the mastoids and middle ears and small ischemic infarction of the right cerebellar hemisphere are also present.
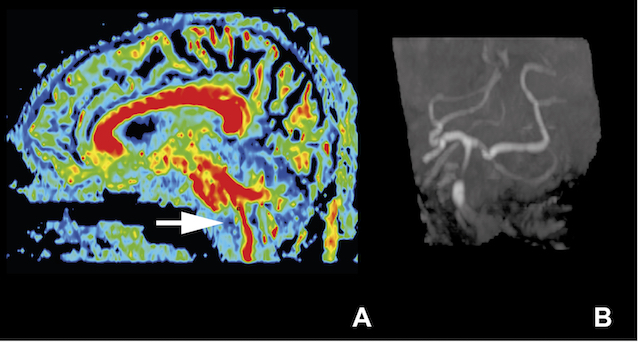
Figure S1. Sagittal reconstructed FA map derived from diffusion tensor imaging (A) and angio MR acquisition of the circle of Willis (B). There is an interruption of the corticospinal track at the junction between the pons and the medulla oblongata (white arrow). The angio MRI discloses a persistent occlusion of the basilar artery at this level, with recirculation in its upper part through the posterior communicating arteries.
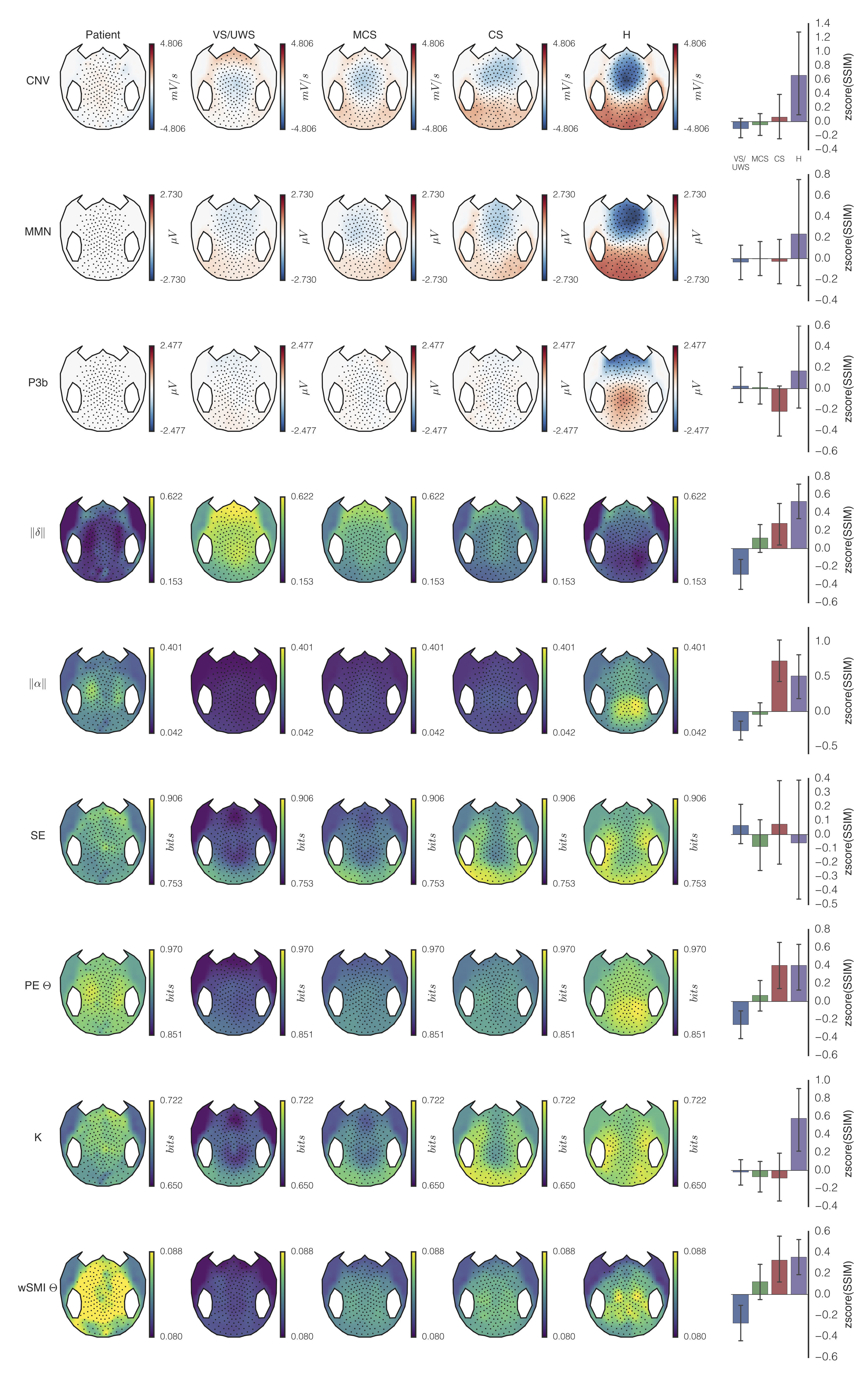
Figure 2. Topographical map of the patient’s EEG markers. Scalp topographical 2D projection (top = front) of each measure [contingent negative variation (CNV), mismatch negativity (MMN), P300b (P3B), normalized power in delta (||δ||) and alpha (||α||) bands, spectral entropy (SE), permutation entropy in theta band (PEθ), Komolgorov-Chaitin Complexity (K) and weighted symbolic mutual information in theta band (wSMIθ)] obtained from the patient’s EEG (first column, “Patient”). These topographies were compared to groups of Vegetative State /Unresponsive Wakefulness Syndrome (VS/UWS: n=76), Minimally Conscious State (MCS; n=68) and Conscious State patients (CS; n=23) as well as Healthy controls (H; n=14). The last column shows the topographical similarity of patient’s topography compared to each of the groups (SSIM; z-score +/- 95%CI).
Reference: Rohaut B, Raimondo F, Galanaud D, Valente M, Sitt J.D, Naccache L. Probing consciousness in a sensory-disconnected paralyzed patient. Brain Injury . 2017 Aug;31:1398-1403. (postprint).