In this review published in Critical Care, we gather current knowledge about consciousness disorders useful for the ICU physician.
We discuss the various terminologies that can be used in the acute setting to describe alterated states of consciousness (Table 1).
Table 1: Definitions of common states of consciousness
Behaviorally defined states:
| Name | Definition | Other terminologies similar or very close |
|---|---|---|
| Coma | State of unresponsiveness in which the patient lies with eyes closed and cannot be aroused to respond appropriately to stimuli even with vigorous stimulation (no eye opening or adapted motor response even to painful stimuli) | Coma-1a or 1b [see note below] (based on EEG compatibility [1a e.g. slow unreactive predominant delta] or not [1b e.g. reactive predominant alpha]). Some authors use a Glasgow coma scale cut-off (e.g., < 8) but this is very misleading since this can include UWS or even MCS patients in whom the ascending reticular activating system (ARAS) is likely to be functional |
| Unresponsive wakefulness syndrome (UWS) | State of unresponsiveness in which the patient shows spontaneous eye opening without any behavioral evidence of self or environmental awareness | Vegetative state (VS), coma vigil, apallic state, UWS/VS-2a or 2b (CMS excluded [2a] or not [2b] by functional MRI or EEG) |
| Minimally conscious state (MCS) | State of severely impaired consciousness with minimal but definite behavioral evidence of self or environmental awareness Distinction between MCS “minus” and “plus” has been proposed [MCS–minus: visual fixation/pursuit or adapted motor reaction to pain; MCS-plus: evidence of language processing (e.g., command following, verbalization…)] | Cortically Mediated State (CMS, in that case CMS-3b as based on behavior alone) |
| Locked-in syndrome (LIS) | State in which the patient is actually conscious but de- efferented, resulting in paralysis of all four limbs and the lower cranial nerves | De-efferented state, Conscious state-4b |
| Conscious state | State of full awareness of the self and one’s relationship to the environment, evidenced by verbal or non-verbal (e.g., purposeful motor behavior) behavior | Exit-MCS (or EMCS) when the patient emerged from MCS, Conscious state-4b |
Brain functional imaging defined states (e.g., fMRI, fEEG, fNIRS, fPET, fMEG):
| Name | Definition | Other terminologies similar or very close |
|---|---|---|
| Higher-order cortex motor dissociation (HMD) | Comatose, UWS or MCS-minus (clinically defined) patients that show association cortex responses to language stimuli | CMS-3a |
| Cognitive motor dissociation (CMD) | Comatose, UWS or MCS-minus clinically defined patients that show MRI or electrophysiologic evidence of command following | Functional locked-in syndrome, Conscious state-4a |
| Communicating-CMD (Com-CMD) | CMD defined patients able to communicate using a brain computer interface (BCI) | Conscious state-4a |
Note: Italic terms refer to the recently proposed Naccache’s terminology. Ranging from 1 to 4, it takes into account both behavioral (“b”) and brain functional imaging (“a”) evidence. Note that as a consequence, the Cortically Mediated State (CMS) and the Conscious state appear both in the behaviorally and the brain functional imaging sections of this table (see original table for more details).
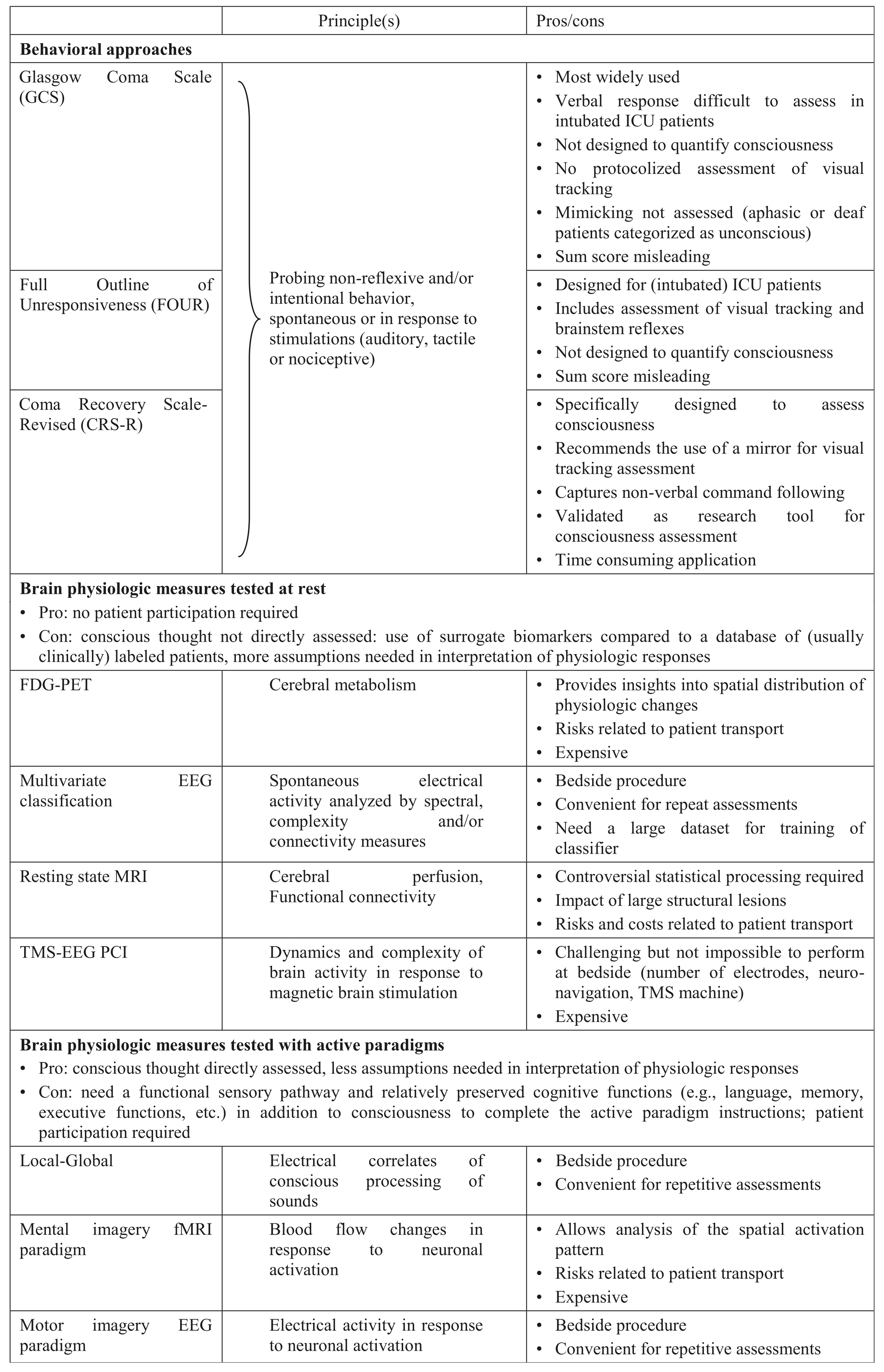
We also summarise and discuss available clinical (i.e. the Glasgow Coma Scale [GCS] the Full Outline of UnResponsiveness [FOUR] score and the Coma Recovery Scale - Revised [CRS-R]) as well as brain imaging techniques (e.g. Local Global paradigm, multivariate resting state EEG analysis, resting state and mental imagery MRI, motor imagery EEG paradigm …) that can be used to assess consciousness in the ICU (Table 2).
(CRS-R: english and french versions)
Table 2: Approaches to assess consciousness in the ICU
Finally, we discuss future Brain Computer Interface (BCI) perspectives for ICU patients.
Reference: Rohaut B, Eliseyev A, Claassen J. Uncovering consciousness in unresponsive ICU patients: technical, medical and ethical consideration. Critical Care. 2019;23(1):78.